Executive Summary
This risk assessment was commissioned in response to an internal audit which required the FSA to update their risk assessment supporting exemptions from microbiological testing in small red meat slaughterhouses. The risk question addressed is: ‘What is the risk to consumers from red meat carcases slaughtered at small throughput slaughterhouses operating under exemption from sampling available in Chapter 3, recital 3.2 of Annex I to Assimilated Regulation (EC) 2073/2005?’
Process Hygiene Criteria define the acceptability, in terms of microbiological safety, of a batch of product before being placed on the market. For red meat carcases, the Process Hygiene Criteria comprise of testing for Salmonella spp., Aerobic Colony Counts and Enterobacteriaceae.
Five size categories of red meat slaughterhouse, based on throughput of red meat species per year, are defined in the FSA’s Manual for Official Controls. The smallest slaughterhouses, size 3, 4 and 5, can currently operate in the UK under the exemption in Assimilated Regulation (EC) 2073/2005 meaning that the smallest (size 5) do not perform any testing, whilst size 3 and 4 are exempt from testing for Salmonella spp. In 2022, the combined annual throughput of these small slaughterhouses, was 5.9% of the total throughput of carcases for cattle, pigs, sheep & goats in England and Wales.
A limited sampling study of 19 red meat slaughterhouses, from all 5 sizes of slaughterhouse (FS900349) was carried out over 6 consecutive weeks in early 2024. This study showed an overall prevalence of 3.2% (15/470) Salmonella spp. in red meat carcases across all sizes of slaughterhouses. No Salmonella was isolated from size 5 slaughterhouses and the prevalence in size 3 and 4 slaughterhouses was 3.6% and 2.1% respectively. This study showed that smaller slaughterhouses who are currently exempted from testing for Salmonella under the Process Hygiene Criteria do not have a higher prevalence of Salmonella spp., than larger slaughterhouses who do currently test. Testing for Enterobacteriaceae and Aerobic Colony Counts indicated that samples from size 5 slaughterhouses, who are exempted from testing, were no more contaminated that those who do test.
Considering the proportion of meat produced in smaller slaughterhouses, and the above study results, these are no riskier than the average slaughterhouse. Of the 8533 cases of salmonellosis reported in England and Wales in 2022, we estimate that no more than 151 arise from consumption of red meat from smaller slaughterhouses who are operating under the exemption.
We have assessed that the overall probability of exposure to consumers from salmonellosis from red meat carcases slaughtered at small throughput slaughterhouses operating under exemption from sampling available in Chapter 3, recital 3.2 of Annex I to Retained Regulation (EC) 2073/2005 is low (rare but does occur). This probability was calculated using the quantitative guidelines in the ACMSF risk representation report.
Lay Summary
This risk assessment estimates the risk to consumers from red meat carcases produced at small throughput slaughterhouses that are exempt from carrying out microbiological sampling. Process Hygiene Criteria define acceptable levels of microbes of a batch of product before being placed on the market. For red meat carcases the Process Hygiene Criteria comprise of testing for different bacteria including Salmonella spp., and hygiene indicator bacteria (Aerobic Colony Counts and Enterobacteriaceae).
Five size categories of red meat slaughterhouse, based on throughput, are defined by the FSA. The smallest slaughterhouses, size 3, 4 and 5, can currently operate in the UK under an exemption in legislation. The smallest (size 5) do not need to perform any testing, whilst size 3 and 4 are exempt from testing for Salmonella spp. In 2022, these smaller slaughterhouses only processed a combined total of 5.9% of all red meat carcases in England and Wales.
A limited sampling study of 19 red meat slaughterhouses (FS900349) was carried out in early 2024. This study showed that 3.2% (15/470) of carcases were contaminated with Salmonella spp. No Salmonella was found in size 5 slaughterhouses. This study found that meat produced by smaller slaughterhouses is no more contaminated with Salmonella spp. than larger slaughterhouses. Testing for hygiene indicator bacteria, found that samples from size 5 slaughterhouses were no more contaminated that those who do test.
Of the 8533 cases of salmonellosis reported in England and Wales in 2022, we estimate that 151 arise from red meat from smaller slaughterhouses who are operating under the exemption. Considering the proportion of meat produced in smaller slaughterhouses, and the above study results, we estimate that small slaughterhouses pose no more risk to consumer health than larger slaughterhouses.
The overall probability of salmonellosis from red meat carcases slaughtered at small throughput slaughterhouses operating under exemption from sampling available in Chapter 3, recital 3.2 of Annex I to Retained Regulation (EC) 2073/2005 is low (rare, but does occur).
Abbreviations
1. Statement of purpose
1.1. Risk Question
What is the risk to consumers from red meat carcases slaughtered at small throughput slaughterhouses operating under the exemptions from sampling available in Chapter 3, recital 3.2 of Annex I to Assimilated Regulation (EC) 2073/2005?
1.2. Scope of risk assessment
This risk assessment will assess the risk to the health of the UK population posed by red meat carcases (cattle, sheep, goats and pigs) from slaughterhouses that are currently exempt from microbiological sampling for Process Hygiene Criteria (PHC) under Assimilated Regulation (EC) 2073/2005 in England and Wales and under EU Regulation (EC) 2073/2005 in Northern Ireland.
Microbiological sampling under the PHC for red meat carcases covers sampling for Enterobacteriaceae, Aerobic Colony Count (ACC) and Salmonella species (spp). Throughput categories and the sampling regimen currently in place for slaughterhouses in England, Wales and Northern Ireland are shown in Table 1. Under Assimilated Regulation (EC) 2073/2005 in England and Wales and under EU Regulation (EC) 2073/2005 in Northern Ireland, small slaughterhouses within the categories 3, 4 and 5 of annual throughput are currently not required to take defined microbiological samples as part of the regulatory PHC, provided this exemption is supported by a risk analysis by the FSA as the Competent Authority. Current exemptions apply to:
-
Category 3 annual throughput 1,500 - 7,500 cattle or horses; 7,500 - 37,500 pigs or sheep/goats. Sampling exemption for Salmonella.
-
Category 4 annual throughput 500 - 1,500 cattle or horses; 2,500 – 7,500 pigs or sheep/goats. Sampling exemption for Salmonella.
-
Category 5 less than 500 cattle or horses; less than 2,500 pigs or sheep/goats. Sampling exemption for all PHC.
Current FSA policy supports small meat processing establishments in applying the exemptions laid out above. This exemption was reportedly based on a historical risk analysis.
However, FSA Policy have identified a need to ensure up-to-date evidence was available to support this policy position and with this in mind, the FSA commissioned this risk assessment.
In scope:
- Red meat slaughterhouses in England, Wales and Northern Ireland.
Out of scope
- Red meat slaughterhouses in Scotland.
Key Assumptions:
-
Data used to inform this risk assessment was collected as part of sampling survey (FS900349) which ran between February/March 2024. We have sampled in the winter and assume this to be a worst-case scenario in terms of animal contamination i.e. dirtier animals in a wet period of weather.
-
Slaughterhouses in the East of England that have been surveyed as part of FS900349 are representative of the rest of England, Wales and Northern Ireland.
1.3. Background
Currently, in the UK, faecal and other contamination of food is assessed against PHC. These criteria define the acceptability of a product or a batch of food to be placed on the market. PHC are applicable only to the food businesses manufacturing, preparing or producing the foodstuff in question. These criteria are set for a product at a specified stage of the process, and they do not apply to products already placed on the market. The results verify whether the food business operators’ (FBO) production processes and their Hazard Analysis and Critical Control Points (HACCP) systems are effectively ensuring compliance with regulatory demands. Failure of a product to meet microbiological standards precipitates investigative activities by the FBO aimed at improving control over processes (Allender, 2020). The FSA, as the Competent Authority, is notified by the business when failure to meet these standards occurs, as corrective action is required. Corrective actions must be documented within procedures based on HACCP principles and good hygiene practices and FBOs are also obliged to investigate the cause of any unsatisfactory results to prevent reoccurrence (FSA, 2023).
Whilst testing isn’t intended to guarantee the safety of batches not tested, these criteria provide objectives and reference points to assist food businesses and Competent Authorities in their activities to manage and monitor the safety of foodstuffs respectively (EFSA, 2005).
1.4. Legislation
Assimilated Commission Regulation (EC) No 2073/2005 (England and Wales) and Commission Regulation (EC) No 2073/2005 (Northern Ireland) on microbiological criteria for foods lays down criteria for relevant foodborne bacteria, their toxins, and their metabolites in various foodstuffs. These criteria define the acceptability of a product, a batch of foodstuffs, or a process, based on the absence, presence or number of microorganisms, and/or on the quantity of their toxins/metabolites, per unit(s) of mass, volume, area or batch, and are applicable to products placed on the market and/or food production processes.
The two different kinds of criteria are defined as follows:
-
Food safety criterion means a criterion defining the acceptability of a product or a batch of foodstuff applicable to products ready to be placed on the market or which are already in the market.
-
Process hygiene criterion means a criterion indicating the acceptable functioning of the production process. It sets an indicative contamination value above which corrective actions are required in order to maintain the hygiene of the process in compliance with food law.
These criteria are, for example, able to indicate whether good hygiene practices are being followed and may assist in understanding whether HACCP procedures are functioning properly. In other words, they are useful for validation and verification of HACCP based processes and procedures. Table 2 shows the PHC for red meat carcases and the action required in case of exceedance of these limits. Of note, pig carcases are permitted a higher level of ACCs and Enterobacteriaceae than other species as carcases remain with skin on. This is to take account of the fact that the skin is inevitably more contaminated, despite scalding, dehairing, singeing, polishing and washing (Zdolec et al., 2022).
2. Hazard identification
Five categories of red meat slaughterhouse are laid out in the FSA’s Manual for Official Controls (chapter 4.1. annex 1) which are based on throughput of species per year. Lower throughput slaughterhouses are either exempt from testing or have a reduced testing schedule (see Table 1). For example, the largest size, category 1, must sample all species every week for 30 weeks (5 swabs per week) for Salmonella spp. Reductions in the frequency or even exemptions from testing can be permitted when based on a risk analysis process carried out by the Competent Authority. A risk assessment was previously carried out by the FSA to assess the risk to the consumer if these exemptions and reductions in frequencies laid out in (Assimilated) Regulation (EC) 2073/2005 were permitted. A recent audit could not locate the risk analysis or risk assessment and therefore there is a need for this work to be commissioned to inform FSA policy teams.
In the UK, approximately 2.3 million tonnes of red meat are produced annually in five different categories of slaughterhouse (comprising: 958,000 tonnes beef, 1,002,000 tonnes pork, and 302,000 tonnes lamb and mutton (Defra, 2022)) of which approximately 25% is exported and an additional 1 million tonnes is imported (Agriculture and Horticulture Development Board (AHDB, 2024)). It is unknown how much meat from each size of slaughterhouse is exported (uncertainty) but for the purposes of this risk assessment it is assumed that meat from those slaughterhouses not testing under the exemption in legislation is not exported. In the UK, the National Diet and Nutrition Survey (NDNS) data shows that an average 6.34 kg of red meat is eaten per person per year (NDNS, 2021).
Raw meat typically has a high water activity (aW) (0.98-0.99) and a slightly acidic to neutral pH of 5.5 to 7, which is conducive for microbial growth (Buncic, 2006). Correct handling, including keeping the cold chain of meat intact, reduces the likelihood of growth of microorganisms within cuts of meat. Cooking of meat thoroughly until the thickest part reaches 70 °C for 2 minutes is sufficient to eliminate Salmonella, E. coli and Enterobacteriaceae. Despite this, foodborne disease is frequently associated with meat. The EFSA zoonosis report (EFSA, 2023) document that for outbreaks with strong evidence linked to food, 20% of outbreaks and 30% of all foodborne disease cases were attributed to meat and meat products (not poultry). The highest cause of meat-related outbreaks and cases in this period was “pig meat and products thereof” (7.1% of outbreaks and 7.4% cases). In contrast, there was strong evidence to link bovine meat and products to only 2.3% of outbreaks and 3.5% of reported cases of human illness, and sheep meat and products to 0.21% of outbreaks and 0.3% of reported cases (EFSA, 2023).
Between July 2023 and June 2024 there were 92 incidents reported to the FSA concerning the presence of pathogenic organisms in meat and meat products, other than poultry. Of these, 71 originated in the UK and Northern Ireland. Most of the incidents concerned minced meat and meat preparations, for example burgers and sausages, rather than carcases. Of the total 92 incidents, 55 (59.7%) identified Salmonella spp., with the remainder involving Shiga-toxin producing Escherichia coli (11 incidents (12%)), Listeria spp., (16 incidents (17.4%)), with the remainder involving species specific viruses (i.e. porcine flu, blue tongue virus) or failure in processing (meaning that processes that are designed to prevent growth of microorganisms have failed or not been validated) (FSA data via the Signals and Incident Management System (SIMS)).
3. Hazard characterisation
3.1. Disease characterisation
Specific microorganisms were chosen in the PHC for specific purposes, e.g. ACC as an indicator of general (and environmental) contamination; Enterobacteriaceae as an indicator of faecal contamination; and Salmonella as the common foodborne pathogen linked to red meat. These organisms therefore represent other pathogens relevant for the respective red meat species. For example, Shiga-toxin producing Escherichia coli (STEC) is relevant for cattle and sheep/goats and Yersinia spp. for pigs. These other pathogens will therefore be considered in this disease characterisation.
3.1.1. Salmonella
Symptoms of Salmonella infection can range from asymptomatic carriage to severe diarrhoea. Children under 10 make up 26% of all Salmonella infections in the UK (UKHSA, 2024a) but infection is usually self-limiting; however, it can be more severe in children under 5 years, the elderly (>65 years) and the immunocompromised (Lund, 2015).
The incubation period of non-typhoidal Salmonella infection is usually between 12-72 hours (CDC, 2024b; UKHSA, 2024a), although periods of up to 144 h (4 to 6 days) are not unusual and incubations of 7 to 9 days and occasionally longer also occur (Eikmier, 2018; Gal-Mor, 2019).
The infectious dose of Salmonella is usually high although this varies between serovars, individuals and food vehicles (Kothary & Babu, 2007). A dose-response model fitted to data from 20 outbreaks gave an estimated ID50 (the pathogen dose likely to cause illness in 50% of test subjects) of approximately 104 cells. High fat foods consumed by vulnerable groups could have an infectious dose as low as 10-100 cells (for instance, consumed dose was estimated to be around 50 cells in a peanut sauce outbreak) (USDA, 2015). An infectious dose of 2.4 x 105 cells was calculated to be responsible for an outbreak of Salmonella Enteritidis from roasted beef at a restaurant, which led to 3 illnesses (World Health Organization & Nations, 2002).
The presence of any Salmonella serovar in RTE foods is considered to be unacceptable and potentially hazardous. However, Salmonella spp. are destroyed by pasteurisation temperatures and the standard 70°C for two minutes cooking advice is sufficient to significantly reduce levels. Salmonella numbers decline upon freezing but cells can remain viable (HPA, 2009).
3.1.2. Aerobic Colony Counts
The Aerobic Colony Count (ACC), also known as the Total Viable Count or Standard Plate Count, is an indicator of hygiene and quality, not safety. It is not considered a risk to human health (HPA, 2009).
3.1.3. Enterobacteriaceae
The Enterobacteriaceae are a family of bacteria, the level of which is used to assess the general hygiene status of a food product and includes species that originate from the intestinal tract of animals and humans, as well as plants and the environment. Enterobacteriaceae are considered useful indicators of contamination with enteric bacteria like E. coli, Salmonella enterica, and some Yersinia spp. Increased counts of Enterobacteriaceae on pig carcasses have been shown to be associated with the occurrence of Salmonella on carcasses (Zdolec et al., 2022).
All Enterobacteriaceae are destroyed by pasteurisation temperatures and the standard 70°C for two minutes cooking advice is normally sufficient to eliminate any Enterobacteriaceae present on food.
3.1.4. Shiga-toxin producing Escherichia coli
Symptoms of STEC infection can be variable, ranging from asymptomatic to diarrhoea, abdominal pain, bloody diarrhoea, and haemolytic uraemic syndrome (HUS). Human factors, such as health, genetics and immune status can affect the severity of outcomes in STEC infections. HUS develops in approximately 10% of patients infected with STEC O157 and is the leading cause of acute renal failure in young children. In a study by Byrne et al. (2020) assessing severity of E. coli O157:H7 they concluded that whilst HUS developed in more children ≤16 years of age, risk for severe disease seems to be lower than for those >16 years of age (Byrne et al., 2020). In the over 60s age group, thrombocytopenia (TTP) (low blood platelets) can also occur. In 2021, 1,151 confirmed cases of STEC were reported in England; children aged 1-4 years old had the highest annual incidence of STEC O157 and children under 1 year old had the highest incidence of STEC non-O157 (UKHSA, 2024c). Worldwide, mortality is generally described as 3-5% (FAO/WHO, 2018) but as discussed above depends on the serotype and virulence genes carried by the STEC. The incubation period is, on average, 3-4 days but can be anywhere between 1-9 days. For most patients, infection is self-limiting, and recovery is seen within 10 days.
The infectious dose for STEC is low although there is uncertainty for strains other than O157:H7. Estimates of dose-response have been made for STEC O157:H7 based on food concentration of the pathogen and patient consumption data from outbreaks, and it is thought that exposure to less than 100 cells of STEC O157:H7 may cause infection. Exposure estimates have been reported from three outbreaks where the concentration of STEC O157:H7 in the food at consumption could be determined; 2 to 45 cells in salami and less than 700 cells in beef patties (FAO/WHO, 2018).
3.1.5. Yersinia spp.
The symptoms of yersiniosis include watery diarrhoea, sometimes with blood in the stool, severe stomach pain, fever and vomiting. Symptoms begin 4 to 6 days after acquiring the bacterium and most people with Yersinia infection recover quickly (within 1 to 3 weeks), often without any treatment. Rarely, Yersinia can cause more severe illness with symptoms lasting up to 8 weeks and require appropriate antibiotics for treatment (CDC, 2024a). The infectious dose is thought to be very high in adults (108−109 cells), but lower in infants and the immunocompromised (Mancini et al., 2022). The numbers of reported cases of yersiniosis in the UK is low, however, this is likely due to under-reporting as it is not routinely screened for in UK laboratories, and in contrast it is the third highest reported cause of gastroenteritis in the EU (EFSA, 2023). A study by Šumilo (2023) estimated that around 7,500 cases of yersiniosis go unreported in England each year (Šumilo et al., 2023) and a study, following the introduction of commercial PCR in a South East hospital laboratory, predicted that the annual incidence was 13.6 cases per 100,000 population in their catchment area between 2017 and 2020 (Clarke et al., 2020).
3.2. Cases, outbreaks and disease attribution studies
Salmonella is one of the main causes of human foodborne illness and is endemic worldwide. In livestock, including poultry, asymptomatic and persistent infection in the animal’s digestive tract results in a carrier state, further facilitating transmission to humans (Cardim Falcao et al., 2024). In studies of human foodborne illnesses, attributing the source of the pathogen is essential for better understanding transmission dynamics and developing efficient control strategies. Salmonella outbreaks are frequently linked to animal reservoirs such as chickens (including table eggs) and pigs. Pinedo et al., (2022) assessed EFSA zoonosis data from 2015-2019 to better understand Salmonella attribution. They found that in Western Europe, the most important food source of salmonellosis outbreaks was “pig meat and products thereof”, which accounted for 18.53% (95% confidence interval (CI) 10.68- 27.84) of human outbreaks attributed to a single source. This was followed by eggs and egg products at 14.73% (95% CI 7.74-23.58) and then “broiler meat (Gallus gallus) and products thereof” at 11.96% (95% CI 5.76-20.08). Bovine meat and sheep meat were attributed to much lower proportions of outbreaks at 2.67% (95% CI 0.34-7.47) and 1.35% (95% CI 0.34 - 7.47) respectively (Chanamé Pinedo et al., 2022).
In England, the single largest cause of outbreaks of Salmonella are associated with the consumption of poultry, followed by other meat products. In 2021-2022, of the outbreaks where a food source was identified, 38% of confirmed cases were attributed to chicken with a further 24% attributed to kebab meat and “meat products” (UKHSA, 2024a). Between 2017 and 2018, a Salmonella outbreak in the UK was associated with consumption of lamb and mutton, with almost 300 cases reported (Almost 300 sick and one dead due to Salmonella in UK | Food Safety News). Another outbreak with 62 cases was associated with lamb in 2019 (UKHSA, 2024b).
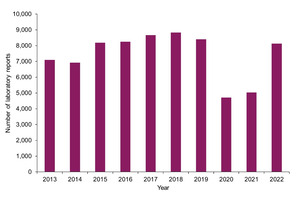
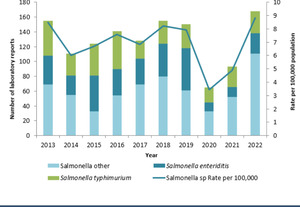
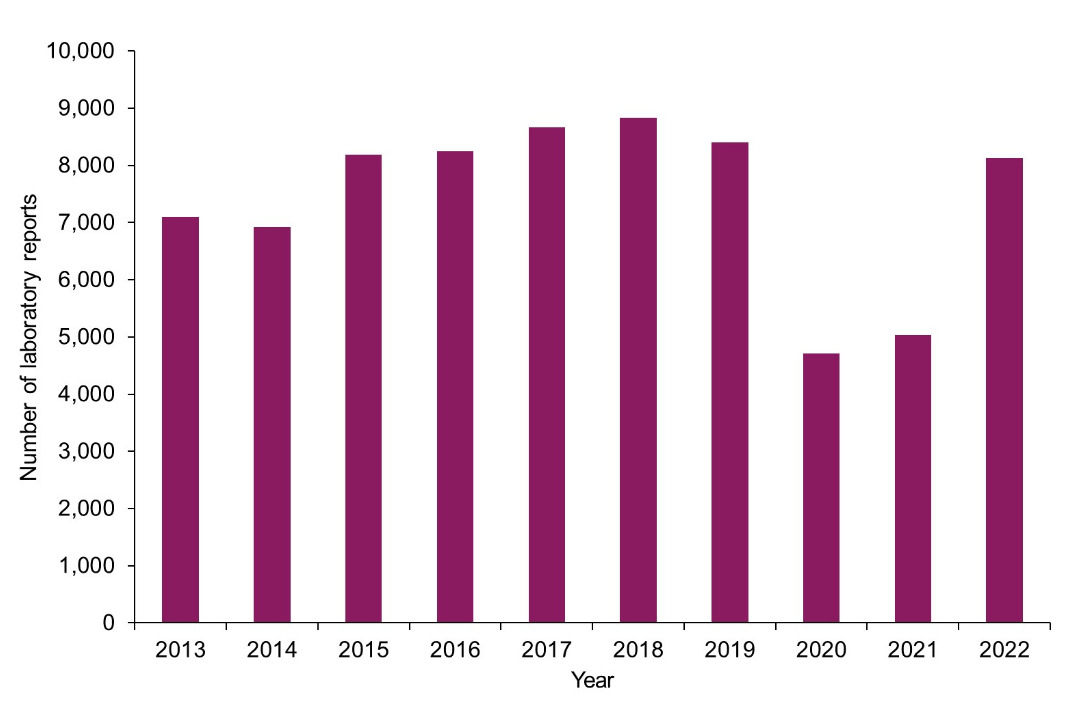
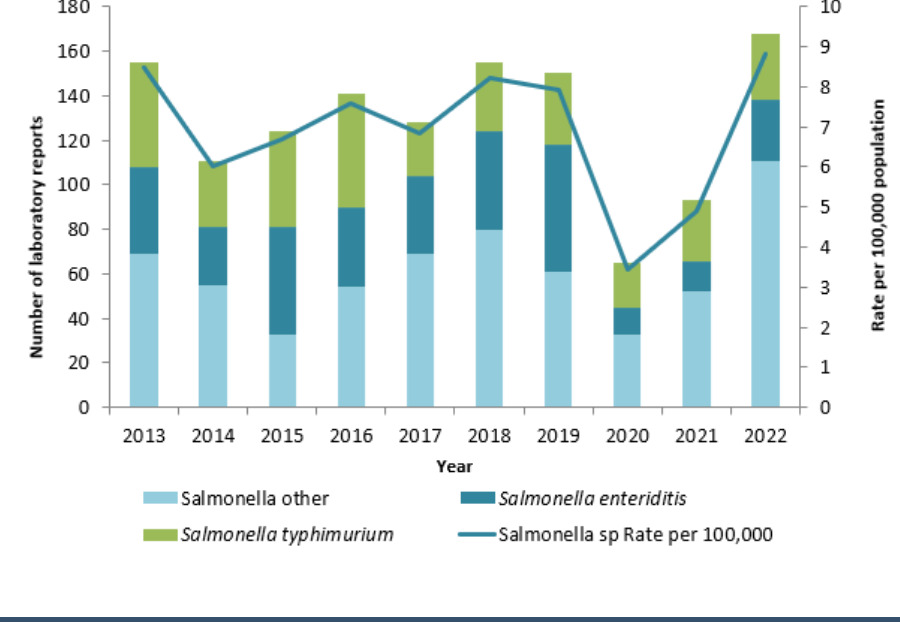
There were 8,704 (UKHSA, 2024a) laboratory-confirmed cases of salmonellosis in England, Wales and Northern Ireland in 2022. The numbers of confirmed cases are generally stable from year to year, with the exception that during the COVID-19 pandemic reported salmonellosis cases fell. Data from 2022 suggests cases have now returned to pre-pandemic levels but there could be multiple reasons behind the fall observed during the pandemic. Love et al., (2021) reviewed the impact of the COVID-19 pandemic on gastrointestinal infection trends in England and noted decreases in gastrointestinal illness across all surveillance indicators at the peak of the pandemic. They concluded that drivers of the changes in reporting of gastrointestinal infections during the first lockdown between February 2020 and July 2020 were likely to be multifactorial; including changes in health seeking behaviour, pressure on diagnostic services and surveillance systems but also that there was a real decrease in the incidence for some pathogens resulting from the control measures and restrictions implemented (Love et al., 2021). The trend in Salmonella cases over the past 10 years is shown in Figure 1 for England (UKHSA, 2024a) and Figure 2 for Northern Ireland (HSCNI, 2024). A similar trend is also observed in Wales (PHW, 2024).
4. Exposure assessment
4.1. Sampling survey
Limited current data are held by the FSA on the levels of contamination in red meat at slaughter in the UK. Although several projects were commissioned in the 2000s, these data are unlikely to accurately reflect current contamination levels. A survey of sheep at slaughter was carried out by APHA and funded by the FSA in 2023/24 (APHA, 2024) but the results were pooled and therefore no information could be extracted to understand the size of slaughterhouse in relation to the results recorded. Therefore, a sampling survey was commissioned to understand contamination levels in slaughterhouses, relevant to the PHC across all sizes of slaughterhouse. This survey aimed to gather evidence to support this risk assessment.
4.1.1. Sampling from low- and high-throughput slaughterhouses
To understand the risk of businesses not sampling in smaller-sized slaughterhouses, it is important to understand the amount of meat that each slaughterhouse size contributes to the market.
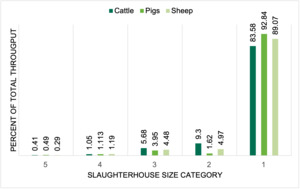
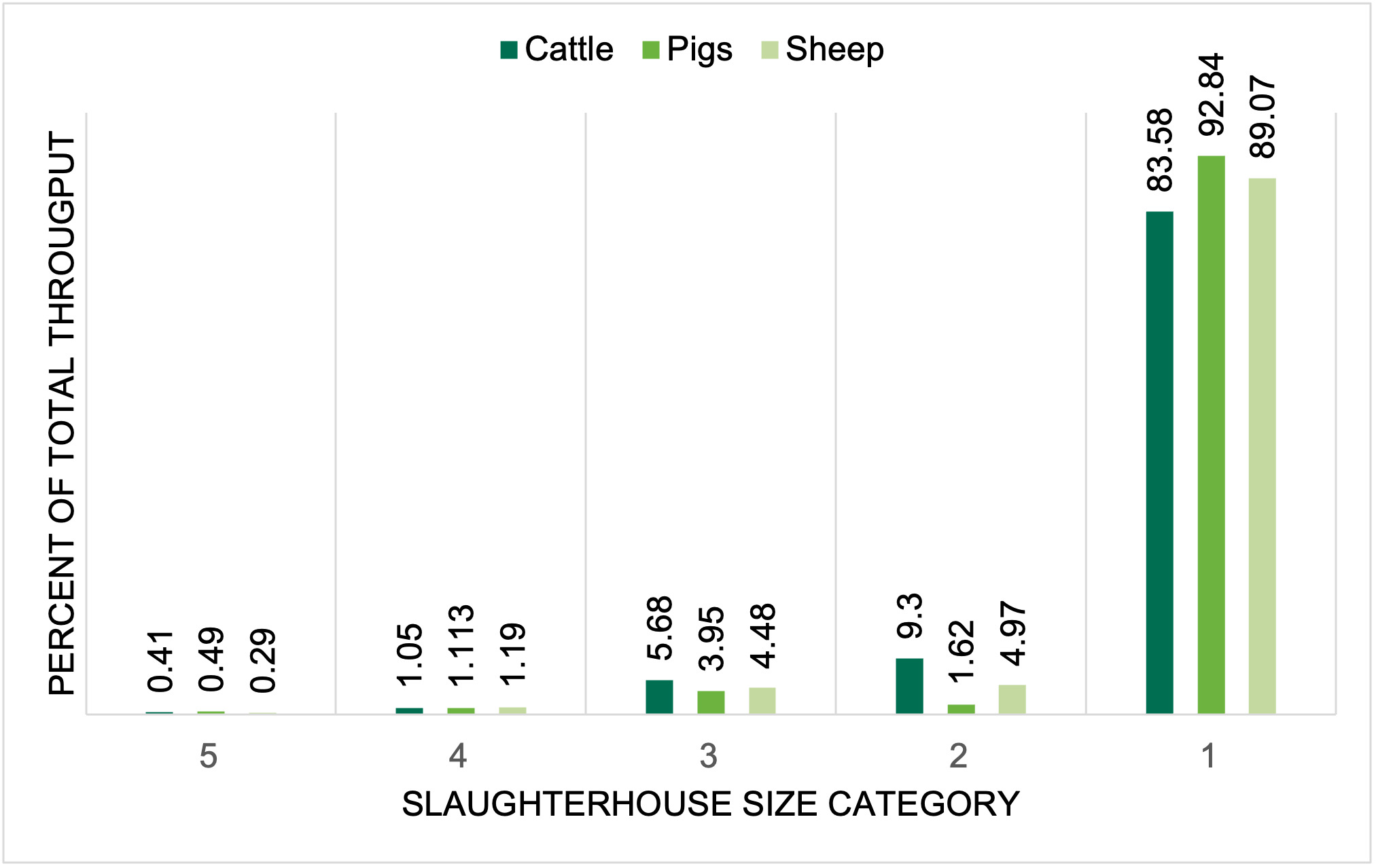
Annual slaughterhouse throughput data (for cattle, sheep and pigs) in establishments based in England and Wales was obtained from FSA operations teams (FSA Operations, Pers. Comm., 2024). Figure 3 shows the percent of throughput per slaughterhouse size for cattle, pigs and sheep in England and Wales. The largest category of slaughterhouse (size 1), process over 80% of the red meat livestock in England and Wales, regardless of species. Size 5 slaughterhouses, the smallest category, process < 0.5% of the total throughput per year across all species. The combined throughput of sizes 3, 4, and 5 slaughterhouses is 5.9% of all red meat animals slaughtered in England and Wales. This information is shown in more detail in Table 3 and Table 4.
As no baseline data for the microbiological contamination of red meat carcases from all sizes of slaughterhouse existed, a small sampling survey was designed to gather data to meet this evidence gap. Due to resourcing restrictions a decision was made, in collaboration with FSA Operations teams and statisticians from the Analytics Unit, to focus on one particular area of England for sampling.
FSA colleagues from the Analytics Unit were consulted to determine an acceptable sample size (FSA Analytics Unit, personal communication, 2023). When determining sample size the following was considered: resource availability in terms of personnel to collect samples, willingness of slaughterhouses to participate, and financial resource. By keeping all slaughterhouses in one geographic region it was felt that this would mitigate any variability in weather during the period of sampling (FSA Analytics Unit, personal communication, 2023). A decision was made to recruit the same number of slaughterhouses in each size category, to allow comparison between the different size categories. Twenty slaughterhouses in the East of England were identified by FSA Operations colleagues and an “opt out” method of recruitment was used. Four slaughterhouses of each throughput size were invited to participate. These were identified by operations colleagues based on close working relationships with the FSA. Species was not considered when recruiting slaughterhouses. All samples were taken by FSA employed staff as per the PHC (Manual for Official controls (FSA, 2024)). Samples were collected post- dressing, pre-chilling and returned to the laboratory (Campden BRI) for testing within 24 hours of sampling. ISO methods were specified to the laboratory for detection and/or enumeration. Species of animal, time of sampling, time of testing and temperature of the transport box contents on arrival in the lab were recorded. All swabs were tested for enumeration of Enterobacteriaceae and ACCs, and presence/absence of Salmonella spp. No further serotyping was carried out.
4.1.2. Results
Of the 20 slaughterhouses approached, 19 agreed to sample for the sampling period. Only 3 slaughterhouses took part from the “size 1” category, one declining to take part via email correspondence but all other sizes had 4 participants. Whilst we requested that five samples per week were taken for 6 consecutive weeks from all 19 establishments, on 4 occasions only 3 samples were submitted and on 2 occasions only 4 were submitted. These slaughterhouses processed sheep and cattle. The reasons for submitting fewer samples are unknown (uncertainty) but could be due to operational reasons such as reduced throughput on that day. The last week of sampling was cut short for operational reasons due to the Easter weekend.
A total of 470 samples were taken of which 44% of samples tested were from sheep, 33% from pig and 23% from cattle. In plants of size 1, 40% of samples tested were from sheep, 30% pig and 30% cattle, while in plants of size 5, 51% of the samples tested were from sheep, 28% pig and 21% cattle suggesting the spread of species was similar for different sizes of slaughterhouse. The data for all slaughterhouse sizes were weighted to match the overall species distribution of samples tested. On this basis, the prevalence of Salmonella across all sizes of slaughterhouses with standard error and 95% confidence intervals were calculated.
The weighted analysis considers the number of samples taken and the number of positives proportionally. We cannot comment further on these results, for example the heterogeneity, due to the low number of positives that were detected during this sampling project (uncertainty).
4.1.2.1. Salmonella
The number of Salmonella-positive swabs over all weeks are shown in Table 5. No Salmonella positives were found in the size 5 category of slaughterhouses, but the highest prevalence is assumed to be 4.1% based on the 95% confidence interval, suggesting that they are still no more contaminated than the larger slaughterhouses. The highest number of positives were in the size 3 category of slaughterhouses at 5.7%, but they also took the greatest number of samples (105). Using weighted analysis (i.e. assessing the proportion of swabs taken from each plant), the highest prevalence was seen in size 2 slaughterhouses at 4.4% (95% CI (0, 8.8)).
Pigs made up 67% (10/15) of all positive Salmonella swabs, but as species of carcase is not in scope for this risk assessment this was not investigated further. However, in light of the EFSA zoonosis report (2023) suggesting that pork is responsible for a significant number of cases of salmonellosis, this could be an area of future interest for the FSA.
The overall prevalence of Salmonella spp., across all sizes of slaughterhouse was found to be 3.2% (15/470 samples were positive). Because no serotyping was undertaken, we do not know if the Salmonella spp., detected were of clinical importance to humans (uncertainty).
Due to the time and budget constraints of the sampling survey no samples were taken in Northern Ireland. However, the EFSA One Health Zoonosis report (2023) suggests that FBO reported Salmonella spp. prevalence in slaughterhouses in Northern Ireland in 2022 was: 1.1% on pig carcases, nil in sheep carcases and 0.06% on cattle carcases (EFSA, 2023). In contrast, for the 24 Member States including Northern Ireland who submitted Competent Authority reported results for carcase contamination, prevalence of Salmonella was as follows: 4.1% in pigs, 1.4% in sheep and 1.4% in cattle. For samples collected by FBOs, the proportion of Salmonella-positive samples was significantly lower: 1.0% for pigs, 0.49% for cattle and 0.76% for sheep (EFSA, 2024). Recent data from a survey of sheep at slaughter in England and Wales carried out by the FSA (APHA, 2024) suggests a prevalence of 0.55% Salmonella on sheep carcases. Essentially, the prevalence of Salmonella from samples taken by the CA seems to be consistently higher than those taken by FBOs. The reason for this is unknown (uncertainty) but highlights the importance of the role of the Competent Authority in the verification of PHC.
The results from this sampling survey suggests that red meat produced in smaller slaughterhouses, size 3, 4 and 5, is no more contaminated with Salmonella spp. than red meat produced in larger slaughterhouses.
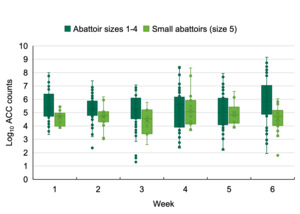
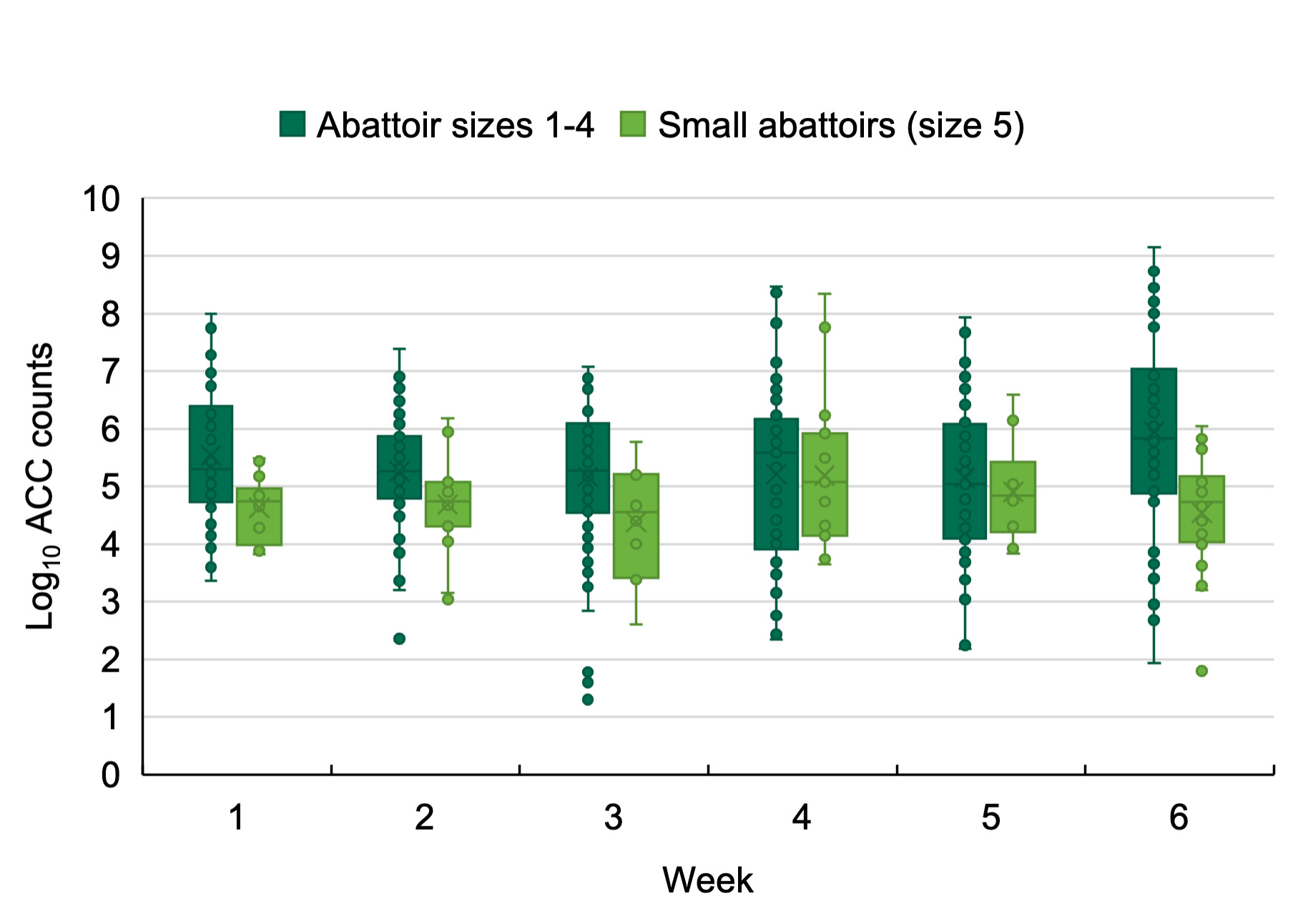
4.1.2.2. Aerobic Colony Counts
Aerobic colony counts were tested for all sizes of slaughterhouses over the sampling period. Figure 4 shows a box and whisker plot of the Log10 of ACCs over the sampling period, comparing size 1-4 slaughterhouses (in dark green) with size 5 only (in light green). The results were analysed for statistical significance using an unpaired 2-way students t-test (see annex 1, Table 8). Over all weeks, except for week 5, ACC counts were significantly lower in size 5 slaughterhouses (p <0.05). At week 5 the results are not significantly different and is not clear why this aberration in the results occurred (uncertainty). Of note, there was little variation over the weeks.
Size 3 and 4 slaughterhouses are not exempt from sampling ACCs and therefore not considered separately.
A number of samples, across all sizes of slaughterhouse, were returned to the laboratory at a temperature of between 8°C and 10°C. Under the PHC sampling plans, the required temperature for return of samples in a maximum of 8°C. This could influence the growth of organisms enumerated as part of the ACC. No other slaughterhouse size except size 5 are exempt from testing for ACCs.
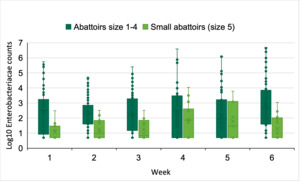
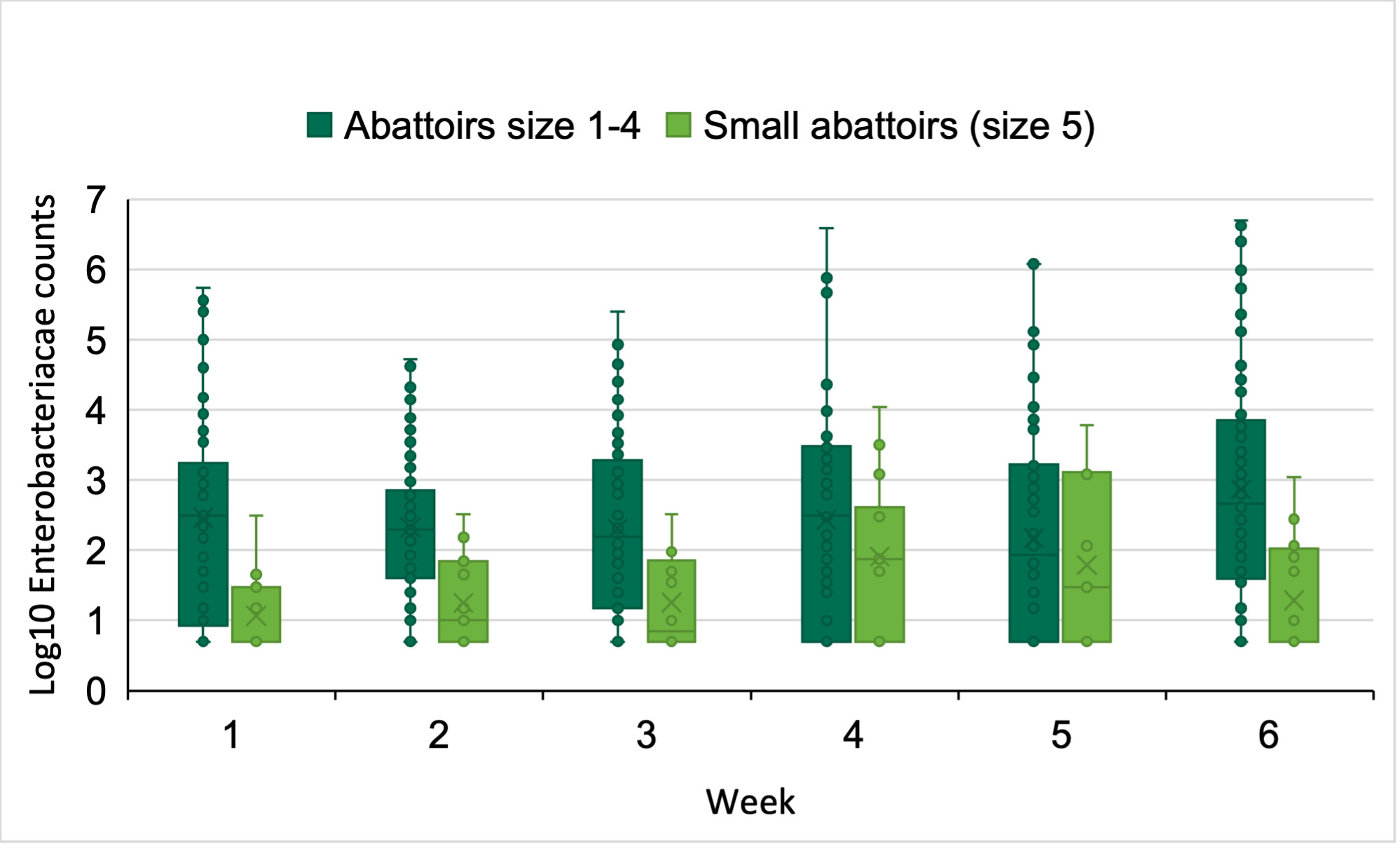
4.1.2.3. Enterobacteriaceae
Enterobacteriaceae counts were collected for all sizes of slaughterhouse over the sampling period. Figure 5 shows a box and whisker plot of the Log10 of Enterobacteriaceae counts over the sampling period, comparing size 1-4 slaughterhouses (in dark green) with size 5 only (in light green). The results were analysed for statistical significance using an unpaired 2-way students t-test (see annex 1). Over weeks 1, 2, 3 and 6, Enterobacteriaceae counts were significantly lower in size 5 slaughterhouses (p <0.05). The counts were not significantly different in weeks 4 and 5, which is a similar trend to that seen with the ACC counts. Because the sample size was smaller, as it only consisted of one size of slaughterhouse, a one off very high count from a carcase could affect the mean counts (uncertainty). There was little variation over the weeks for the size 1-4 slaughterhouses. Enterobacteriaceae counts were more varied over time for the size 5 slaughterhouses. The reason for this is unknown (uncertainty).
A number of samples, across all sizes of slaughterhouse, were returned to the laboratory at a temperature of between 8°C and 10°C. Under the PHC sampling plans, the required temperature for return of samples in a maximum of 8°C. This could influence the growth of Enterobacteriaceae.
4.2. Limitations of sampling
The application of microbiological criteria has certain limitations. Due to reasons related to sampling, methodology and uneven distribution of micro-organisms, microbiological testing alone can never guarantee the safety of a foodstuff tested. Therefore, the safety of foodstuffs is principally ensured by a structured preventive approach, such as good product and process design and the application of good hygiene practice and the Hazard Analysis Critical Control Point (HACCP) principles. If no action is taken due to failed or unsatisfactory results, then sampling alone does not make any difference to the safety of the meat.
There are limitations of the sampling survey that took place for this project, and it is accepted that there are uncertainties that weren’t controlled for in this work. For example, size 1 slaughterhouses are likely highly mechanized suggesting less variability between plants whilst variability of size 5 slaughterhouses would be expected to be high for example due to variances in layout and practices (uncertainty). However, as the FSA had previously held limited current data on the PHC results between different sizes of slaughterhouses we feel that the results of the sampling survey were applicable to this risk assessment.
4.3. Total exposure of UK consumers to meat contaminated with Salmonella spp.
Using the data collected in FS900349 and as explained in section 3 we can assume that a portion of meat from a smaller slaughterhouse is no riskier than that from larger slaughterhouses. The throughput of red meat carcases in small slaughterhouses is only 5.9% of the total throughput in England and Wales. 30% of reported Salmonella cases are attributable to red meat (EFSA, 2023). Assuming all red meat from small slaughterhouses stays for consumption in the UK, of the 8533 reported cases of salmonellosis in England and Wales in 2022, we estimate that 151 reported cases will be attributable to red meat from these smaller slaughterhouses. In this calculation we assume that imported meat is similarly as risky as UK produced meat. When considering only size 5 slaughterhouse: 0.38% of UK slaughtered red meat is produced by these establishments; using the same calculation as above we estimate 10 cases of salmonellosis being attributed to them. For size 4 (who process 1.15 % of the red meat throughput) this number is 29 cases and for size 3, the largest category of smaller slaughterhouses (processing 4.36% of the throughput) this increases to 112 cases. The population of England and Wales was reported as 60,240,000 in 2022 (ONS, 2024). Table 6 shows the estimated cases per 100,000 population in England and Wales for size 3, 4 and 5 slaughterhouses, and all three sizes combined. Although data for Northern Ireland is not included in these calculations, we assume the proportion of throughput in different size slaughterhouses is similar and therefore the same case estimation would apply (uncertainty).
4.4. Action taken as a result of an exceedance
Currently, no specific enforcement actions are taken as a result of slaughterhouses failing to sample or failing the PHC requirements (Gherman et al., 2022). Interventions are left to the discretion of the slaughterhouse to review their HACCP and investigate trends in unsatisfactory results although it should be noted that major retailers can apply pressure on businesses to supply them with meat that has low levels of microbiological contamination (D. Antic, personal communication, 2022). However, if the smallest slaughterhouses are not sampling then, of course, no action can be taken.
There were limited data to assess differences in the PHC levels between carcases being processed by low- and high-throughput slaughterhouses. Furthermore, although data were gathered on the levels of contamination after slaughter but before retail, no data was gathered on the actions that would be taken as a result of exceeding a target threshold. In addition, the data were collected over a limited period of 6 weeks from 8th February to 21st March 2024 and may not be fully representative. We aimed to minimise this limitation by taking samples from all categories and from the same area, geographically, of the UK, so that we are comparing like-for-like across size categories. All reported cases of non-typhoidal Salmonella, regardless of serovar, peak in late summer/early autumn (UKHSA, 2018) so prevalence may be higher at different times of the year. We sampled from slaughterhouses of different sizes while controlling for region and time of year to minimise the risk of systematic biases due to seasonal effects. The fact that we were only able to sample from a limited geographical region and during a restricted time period does not allow us to conclude with certainty that more extreme differences might be seen if the study was repeated at different times of the year or from a different region. However, because all sizes of slaughterhouse were considered in this assessment, we feel that the risk of this is mitigated.
5. Risk Characterisation
The aim of this risk assessment was to examine how sampling frequency in low-throughput slaughterhouses, i.e., throughput categories 3-5, affect the risk of these two sampling scenarios:
- Size 5 not sampling within the PHC
- Size 3 and 4 slaughterhouses sampling for Enterobacteriaceae and ACCs but not for Salmonella
Sampling does not directly impact public health unless it triggers control measures that are effective at reducing the frequency or level of microbiological contamination. When unsatisfactory results are detected under the PHC, there are recommendations that corrective actions occur, implemented by the FBO, which includes trend analysis of the results and has the aim to improve future production (FSA, 2024). If no testing is undertaken at low-throughput slaughterhouses the probability of taking voluntary actions as a result of unsatisfactory results is automatically zero, although action may be taken for other reasons.
Analysis of the incidents reported to the FSA in the year between July 2023 and June 2024 suggests that whilst Salmonella is the most commonly reported pathogen in meat other than poultry, only a very small proportion of these incidents are likely directly linked to meat carcases from slaughterhouses.
Size 5 slaughterhouses, the smallest category under the Manual of Official Controls (chapter 4) produce less than 0.4% of all the red meat carcases produced in England and Wales. The results from our limited survey suggested that they produced meat that was less contaminated in terms of ACCs and Enterobacteriaceae counts over the sampling period. No samples tested positive for Salmonella spp., from size 5 slaughterhouses during our survey. The worst-case level of Salmonella prevalence in size 5 slaughterhouses is estimated to be 4.1%, which is no worse than the largest slaughterhouses, which contribute the most red meat to the UK market.
Salmonella spp., ACC’s and Enterobacteriaceae, and the pathogens that these organisms act as proxy for, are all readily destroyed by temperatures of 70 °C for a 2-minute period and therefore adequate cooking and hygiene handling would mitigate the risks of any pathogens present.
Therefore, the impact on consumer health by allowing these slaughterhouses not to sample under the PHC is unlikely to result in a significant risk of illness in the UK population. Considering Salmonella spp., we estimate that the probability of exposure for UK consumers to meat produced from this smallest size of slaughterhouse is negligible (so rare it does not merit to be considered). This probability was calculated using the quantitative guidelines in the ACMSF risk representation report.
There is also the probability of exposure to other hazards, represented by ACC and Enterobacteriaceae. However, from our limited sampling study we showed that size 5 slaughterhouses are no more contaminated with these indicator organisms, in fact are significantly less contaminated in 5 out of 6 weeks tested, than larger slaughterhouses.
We only sampled from one geographic area of the UK over a 6-week period due to time and budget restraints, but we assume that a similar picture is seen throughout the UK. This risk assessment is based only on a small sampling survey over a short period in the winter. We have implicitly assumed that all human salmonellosis cases, attributable to red meat, are attributable to UK produced red meat, as we have no data on the prevalence in imported meat. We have therefore assumed a worst-case scenario in this risk assessment. This probability is given with medium uncertainty. Medium uncertainty is defined as there are some but no complete data available; evidence is provided in a small number of references; authors report conclusions that vary from one another.
Under the derogation, size 3 and 4 slaughterhouses must still sample for ACCs and Enterobacteriaceae but testing for Salmonella spp. is not required. Size 3 and 4 slaughterhouses produce more meat than the smallest size 5 establishments but only a combined total of 5.5% across all species.
Size 4 slaughterhouses process 1.15% of the total throughput in England and Wales. Although the contamination of carcases with Salmonella spp. appears more than in size 5 slaughterhouses (3/102 positives samples in our limited study) when the weighted analysis is considered there is no significant difference in the level of Salmonella spp. contamination. The worst-case estimate of prevalence of Salmonella spp. is 4.5% suggesting that Salmonella prevalence in red meat is no higher than in size 1 and 2 (6.2% and 8.5%, respectively). Salmonella spp., and the pathogens this is a proxy for, are all readily destroyed by temperatures of 70 °C for a 2-minute period and therefore adequate cooking and hygiene handling would mitigate the risks of any pathogens present. We estimate the probability of exposure to the UK population of salmonellosis from red meat produced in slaughterhouses from size 4 exempted from Salmonella testing to be very low (very rare but cannot be excluded). This probability was calculated using the quantitative guidelines in the ACMSF risk representation report.
We only sampled from one geographic area of the UK over a 6-week period due to time and budget restraints, but we assume that a similar picture is seen throughout the UK. We have implicitly assumed that all human salmonellosis cases, attributable to red meat, are attributable to UK produced red meat, as we have no data on the prevalence in imported meat. We have therefore assumed a worst-case scenario in this risk assessment. This probability is given with medium uncertainty. Medium uncertainty is defined as there are some but no complete data available; evidence is provided in a small number of references; authors report conclusions that vary from one another.
The probability of exposure as per the ACMSF risk representation report (2020) is summarised in Table 7.
Size 3 slaughterhouses process 4.4% of the total throughput in England and Wales. The contamination of carcases with Salmonella spp. appears more than in size 4 and 5 slaughterhouses (6/105 positives samples in our limited study). When the weighted analysis is considered, there is no significant difference in the level of Salmonella spp. contamination. The worst-case estimate of prevalence of Salmonella is 6.2% suggesting that Salmonella spp. prevalence in red meat is no higher than in size 1 and 2 (6.2% and 8.5%, respectively). Salmonella spp. and the pathogens this is a proxy for, are all readily destroyed by temperatures of 70°C for a 2-minute period and therefore adequate cooking and hygiene handling would mitigate the risks of any pathogens present. We estimate the probability of exposure of the UK population to Salmonella from red meat produced in size 3 slaughterhouses to be low (rare but does occur). This probability was calculated using the quantitative guidelines in the ACMSF risk representation report.
In contrast we estimate that the probability of exposure to the UK population from red meat produced in size 1 and 2 slaughterhouses who process a combined throughput of 94.1% of all red meat to be medium (occurs regularly). This probability was calculated using the quantitative guidelines in the ACMSF risk representation report.
We only sampled from one geographic area of the UK over a 6-week period due to time and budget restraints, but we assume that a similar picture is seen throughout the UK. We have implicitly assumed that all human salmonellosis cases, attributable to red meat, are attributable to UK produced red meat, as we have no data on the prevalence in imported meat. We have therefore assumed a worst-case scenario in this risk assessment. This probability is given with medium uncertainty. Medium uncertainty is defined as there are some but no complete data available; evidence is provided in a small number of references; authors report conclusions that vary from one another.
The severity of detriment of salmonellosis is considered to be medium. “Medium” is interpreted as moderate illness: incapacitating but not usually life-threatening, sequelae rare, moderate duration (e.g. diarrhoea requiring hospitalisation).
We have assessed that the overall probability of exposure to consumers from salmonellosis from red meat carcases slaughtered at small throughput slaughterhouses operating under exemption from sampling available in Chapter 3, recital 3.2 of Annex I to Retained Regulation (EC) 2073/2005 is low (rare but does occur). This probability was calculated using the quantitative guidelines in the ACMSF risk representation report.
Because this risk assessment is based only on a small sampling survey over a short period in the winter, we have no further typing of the positive Salmonella isolates and we do not have information on the role of imported meat on human salmonellosis cases, this risk is given with medium uncertainty. Medium uncertainty is defined as there are some but no complete data available; evidence is provided in a small number of references; authors report conclusions that vary from one another.
5.1. Uncertainties
-
The assumption that slaughterhouses in the East of England are broadly representative of the rest of England, Wales and Northern Ireland. If this is not the case, then the conclusions of the risk assessment may well differ, if it is found that the prevalence of Salmonella and general hygiene indicators are higher in smaller slaughterhouses.
-
Throughput in different sizes of slaughterhouses in Northern Ireland follows the same distribution as in England and Wales.
-
Meat production is seasonal and the sampling survey to inform this risk assessment took place in a quieter time of year. Human cases of salmonellosis peak in the summer (UKHSA, 2024a). However, we have assumed that the differences in level of contamination of meat from each slaughterhouse sizes are distributed similarly over the year.
-
Clinical significance of positive results is unknown e.g. serotypes of Salmonella were not typed so pathogenicity is unknown. However, results from a recent survey of sheep at slaughter in England and Wales (APHA, 2024), suggests that majority of isolates from sheep are S. diarizonae, a sheep adapted pathogen that is generally not associated with human outbreaks. If Salmonella spp. were typed, a better estimate of the impact that meat and meat products have on human salmonellosis cases.
-
We do not know what role imported red meat plays in salmonellosis cases in humans. This risk assessment assumes all reported salmonellosis cases are attributed to red meat produced in England and Wales. Information on the prevalence of Salmonella on red meat that is imported into the UK would meet this evidence gap.